Multiple Myeloma
|
|
Multiple Myeloma
|
|
Pneumothorax
Tension Pneumothorax |
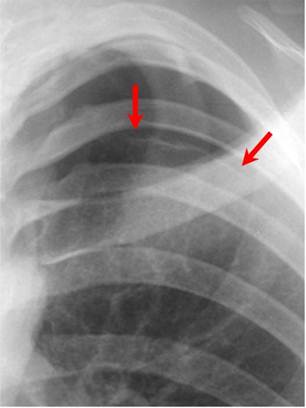
Red arrows point to thin white visceral pleural line which
is the single best sign for a pneumothorax
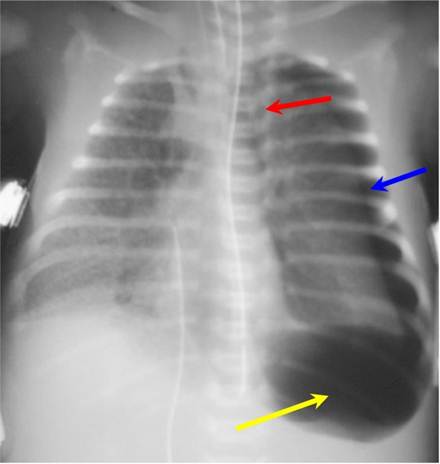
Tension pneumothorax on left (blue arrow) is displacing the heart and mediastinal structures to the right (red arrow);
this case also shows a deep sulcus sign on the left (yellow arrow). There is underlying hyaline membrane disease.
|
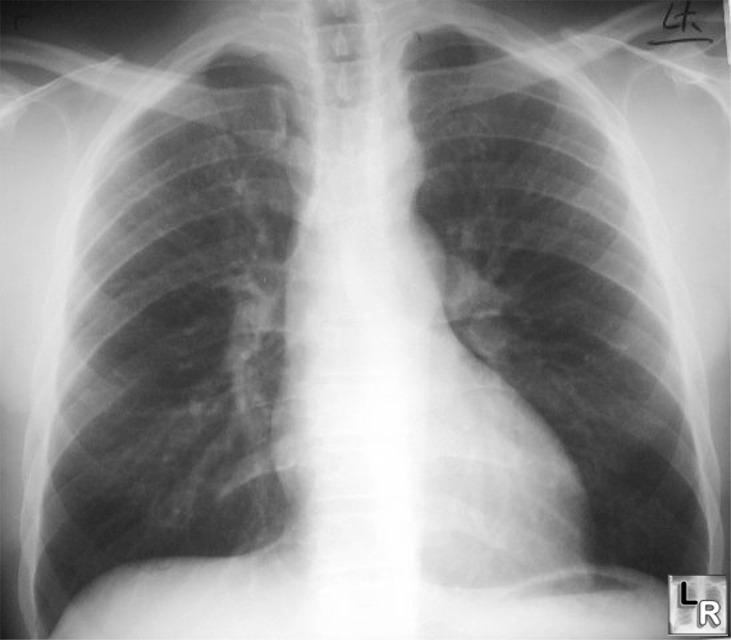
Tension Pneumothorax. Radiograph of the chest shows a large left-sided pneumothorax (white arrows) which is under tension as manifest as displacement of the heart to the right (black arrow) and depression of the left hemidiaphragm (yellow arrow).
|
Tuberculosis
§ Upper lobes affected slightly more than lower
§ Alveolar infiltrate
§ Cavitation is rare
§ Lobar pneumonia is almost always associated with lymphadenopathy—therefore, lobar pneumonia associated with hilar or mediastinal adenopathy at any age should strongly suggest TB
§ Mostly unilateral hilar and/or paratracheal, usually right sided, rarely bilateral
§ Differentiates primary from postprimary TB—it does not occur in postprimary TB
§ Much more common in children
· Airway
· Atelectasis classically affects the anterior segments of the upper lobes or the medial segment of the RML
· Pleura
§ Pleural effusion as a manifestation of primary TB occurs more often in adults than children
§ With appropriate treatment, it carries the best prognosis of all patterns of TB and is the least likely to develop complications
§ The fluid accumulates slowly and painlessly—therefore, patients with TB are seldom seen with a small amount of pleural fluid
§ Parenchymal disease will almost never be present with a pleural effusion although lymphadenopathy may
§ Apical pleural scarring is rarely tuberculous in origin
Postprimary Tuberculosis (“Reactivation TB”)
Patterns of distribution
§ Almost always affect the apical or posterior segments of the upper lobes or the superior segments of the lower lobes—bilateral upper lobe disease is very common
§ May present as pneumonia
§ Cavitation may result: the cavity is usually thin-walled, smooth on the inner margin with no air-fluid level
§ Transbronchial spread may occur—from one upper lobe to opposite lower or to another lobe
§ Miliary spread (below)
§ Bronchiectasis—usually asymptomatic
§ Bronchostenosis due to fibrosis and stricture: fibrosis may cause distortion of a bronchus and atelectasis many years after the initial infection—“middle lobe syndrome”
§ Solitary pulmonary nodule—the tuberculoma—may occur in either primary or postprimary disease; round or oval lesions with small, discrete shadows in the immediate vicinity of the lesion—the “satellite” lesion
Miliary Tuberculosis
TB and Other Diseases
HIV and TB
|